Depression
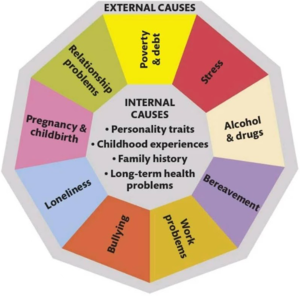
Depression is a form of mental illness which is characterised by a negative cognitive bias resulting in depressed mood, loss of interest in activities, or cognitive impairment[1]. The causative factor(s) of the disease may be external via the environment (exogenous) or internal via a neurochemical imbalance (endogenous) (see Figure 1).
Diagnosis
Diagnosis of depression was traditionally performed by a psychiatrist, however due to an undue amount of human error[2][3][4]in the modern day this has shifted to algorithmic psychometric tests. New developments in the field have shown the efficacy of using voice[5] and facial recognition[6] technology to further aid diagnosis.
Treatment
Depression may be a natural reaction to the environment. To treat the disease, external factors should be eliminated first, then endogenous issues should be explored. The main points to initially address are:
- Healthy diet - supplementation of Vitamin D3, tryptophan[7] and Omega 3, ↓ alcohol consumption.
- Sunlight - running outside as below can bolster Vitamin D3 as above.
- Exercise - 3+ times a week, the higher the intensity the better, best activity is to run in nature[8][9].
- Sleeping well - by exposing yourself to sunlight you can reset your Circadian Rhythm whilst exercising can also help you sleep.
- Reducing overstimulation - anti rumination, reduce caffeine intake do more mindfulness and meditation.
- Talking - self therapy, counselling, increase social contact.
The next step would be to consider a antidepressant. Doctors often prescriber the SSRI, fluoxetine as the first port of call however statistically, they (and all other antidepressants) are only effective by a small margin. It has been found that 54% of adults experience a reduction in symptoms after taking an antidepressant, however 35–40% experience similar improvements after taking a placebo. This means antidepressants are only responsible for a decrease in symptoms of around 20%[10]. To compound this, the 20% who see some effectiveness are plagued by the fact that about a third of these symptoms return at some point during therapy.
Relapse
People who have recovered from an episode of depression (whether spontaneously or following the provision of treatment) are at an increased risk of becoming depressed again in the future. This risk can be as high as 60% for people who have experienced one episode, 70% in those who have had two episodes, and 90% in those who have had three previous episodes (American Psychiatric Association, 2000). Psychological therapies delivered following recovery from depression, including CBT, MBCT, and IPT, may reduce risk of relapse after one year by 22%[11].
References
- ↑ The association between overweight/obesity and poor cognitive function is mediated by inflammation in patients with major depressive disorder. Xiaofeng Lan, Chengyu Wang, Weicheng Li, Ziyuan Chao, Guohui Lao, Kai Wu, Guixiang Li, Yuping Ning, Yanling Zhou, Journal of Affective Disorders, Volume 313, 2022, Pages 118-125,https://doi.org/10.1016/j.jad.2022.06.073.
- ↑ Rates of Detection of Mood and Anxiety Disorders in Primary Care: A Descriptive, Cross-Sectional Study Monica Vermani, PsyD, Madalyn Marcus, MA. Prim Care Companion CNS Disord. 2011; 13(2): PCC.10m01013. doi: 10.4088/PCC.10m01013. Accessed on 30th November 2022 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3184591/
- ↑ Analysis of Misdiagnosis of Bipolar Disorder in An Outpatient Setting. Shen H, Zhang L, Xu C, Zhu J, Chen M, Fang Y. Shanghai Arch Psychiatry. 2018 Apr 25;30(2):93-101. doi: 10.11919/j.issn.1002-0829.217080. PMID: 29736129; PMCID: PMC5936046. Accessed on 30 November 2022 via: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936046/
- ↑ Beyond Misdiagnosis, Misunderstanding and Mistrust: Relevance of the Historical Perspective in the Medical and Mental Health Treatment of People of Color. Derek H. Suite, MD, MS; Robert La Bril, MDiv; Annelle Primm, MD, MPH; and Phyllis Harrison-Ross, MD. Accessed on 30 November 2022 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2574307/pdf/jnma00207-0025.pdf
- ↑ Detecting subtle signs of depression with automated speech analysis in a non-clinical sample. König, A., Tröger, J., Mallick, E. et al. BMC Psychiatry 22, 830 (2022). https://doi.org/10.1186/s12888-022-04475-0.
- ↑ Diagnosis of Depressive Disorder Model on Facial Expression Based on Fast R-CNN. Diagnostics (Basel). Lee YS, Park WH. 2022 Jan 27;12(2):317. doi: 10.3390/diagnostics12020317. PMID: 35204407; PMCID: PMC8871079.
- ↑ The effects of dietary tryptophan on affective disorders. Arch Psychiatr Nurs. 2015 Apr;29(2):102-7. doi: 10.1016/j.apnu.2014.11.008. Lindseth G, Helland B, Caspers J. Epub 2014 Dec 9. PMID: 25858202; PMCID: PMC4393508. Accessed on 30 Jan 2023 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4393508
- ↑ Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Ben Singh, Timothy Olds, Rachel Curtis, University of South Australia, Adelaide, Australia; Accessed on 31 March 2023 via the BMJ http://orcid.org/0000-0002-7227-2406
- ↑ The effects of walking in nature on negative and positive affect in adult psychiatric outpatients with major depressive disorder: Kia Watkins-Martin, Despina Bolanis, Stéphane Richard-Devantoy, Marie-Hélène Pennestri, Catherine Malboeuf-Hurtubise, Frederick Philippe, Julie Guindon, Jean-Philippe Gouin, Isabelle Ouellet-Morin, Marie-Claude Geoffroy, A randomized-controlled study, Journal of Affective Disorders, Volume 318, 2022,Pages 291-298, ISSN 0165-0327, https://doi.org/10.1016/j.jad.2022.08.121.
- ↑ Treatment outcomes for depression: challenges and opportunities. Pim Cuijpers, Argyris Stringaris, Miranda Wolpert. Published in the Lancet Psychiatry: February 17, 2020. Accessed on 31 March 2023 via DOI:https://doi.org/10.1016/S2215-0366(20)30036-5
- ↑ Can non-pharmacological interventions prevent relapse in adults who have recovered from depression? A systematic review and meta-analysis of randomised controlled trials. Clinical Psychology Review. Volume 39, July 2015, Pages 58-70