Depression: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| (One intermediate revision by the same user not shown) | |||
| Line 3: | Line 3: | ||
=== Diagnosis === | === Diagnosis === | ||
The diagnosis of depression has traditionally been conducted by psychiatrists or doctors. However, to reduce human error<ref>'''Rates of Detection of Mood and Anxiety Disorders in Primary Care''': A Descriptive, Cross-Sectional Study Monica Vermani, PsyD, Madalyn Marcus, MA. Prim Care Companion CNS Disord. 2011; 13(2): PCC.10m01013. doi: 10.4088/PCC.10m01013. Accessed on 30th November 2022 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3184591/</ref><ref>'''Analysis of Misdiagnosis of Bipolar Disorder in An Outpatient Setting'''. Shen H, Zhang L, Xu C, Zhu J, Chen M, Fang Y. Shanghai Arch Psychiatry. 2018 Apr 25;30(2):93-101. doi: 10.11919/j.issn.1002-0829.217080. PMID: 29736129; PMCID: PMC5936046. Accessed on 30 November 2022 via: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936046/</ref><ref>'''Beyond Misdiagnosis, Misunderstanding and Mistrust: Relevance of the Historical Perspective in the Medical and Mental Health Treatment of People of Color'''. Derek H. Suite, MD, MS; Robert La Bril, MDiv; Annelle Primm, MD, MPH; and Phyllis Harrison-Ross, MD. Accessed on 30 November 2022 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2574307/pdf/jnma00207-0025.pdf</ref> , there has been a growing shift towards using algorithmic psychometric tests based on yes/no or rating-scale questionnaires. Emerging advancements in the field suggest that voice<ref>'''Detecting subtle signs of depression with automated speech analysis in a non-clinical sample.''' König, A., Tröger, J., Mallick, E. ''et al.'' ''BMC Psychiatry'' 22, 830 (2022). https://doi.org/10.1186/s12888-022-04475-0.</ref> and facial recognition technology<ref>'''Diagnosis of Depressive Disorder Model on Facial Expression Based on Fast R-CNN. Diagnostics''' (Basel). Lee YS, Park WH. 2022 Jan 27;12(2):317. doi: 10.3390/diagnostics12020317. PMID: 35204407; PMCID: PMC8871079.</ref> could play a significant role in enhancing diagnostic accuracy in the future. | |||
=== Cognitive Biases === | === Cognitive Biases === | ||
[[Cognitive biases]] are believed to be both a root cause and a symptom of depression, with two primary biases playing a significant role. The first is [[Attention Bias|attention bias]], where the mind becomes unconsciously conditioned to focus on negative external stimuli. The second is [[Negativity Bias|negativity bias]], which involves a tendency to dwell on negative internal thoughts—such as past regrets or future anxieties—as well as unfavorable aspects of the surrounding environment. | |||
Attention acts as a filter, determining which information from our internal thoughts and external environment is processed further<ref>Woody, M. L., Rohac, R., Cooper, I., Griffo, A., McDonald, N., Spotts, C., Fournier, J., Jones, N., Peciña, M., Young, K., Shivanekar, S., Rengasamy, M., Grafton, B., & Price, R. B. (2024). '''The Impact of Intravenous Ketamine on Attentional Bias: Probing Mechanisms of Rapid-Acting Antidepressant Effects Across Two Clinical Studies'''. ''Biological Psychiatry''. <nowiki>https://doi.org/10.1016/j.biopsych.2024.10.024</nowiki></ref>. People with depression often show a tendency to focus more on negative environmental information while ignoring neutral or positive details. This biased attention leads to an imbalanced integration of information across cognitive systems, resulting in predominantly negative memories, interpretations of events, and perceptions of the self, others, and the world. Over time, this creates a self-reinforcing cycle, where the focus on negative information perpetuates depressive thoughts and feelings, sustaining the depressed mood. | Attention acts as a filter, determining which information from our internal thoughts and external environment is processed further<ref>Woody, M. L., Rohac, R., Cooper, I., Griffo, A., McDonald, N., Spotts, C., Fournier, J., Jones, N., Peciña, M., Young, K., Shivanekar, S., Rengasamy, M., Grafton, B., & Price, R. B. (2024). '''The Impact of Intravenous Ketamine on Attentional Bias: Probing Mechanisms of Rapid-Acting Antidepressant Effects Across Two Clinical Studies'''. ''Biological Psychiatry''. <nowiki>https://doi.org/10.1016/j.biopsych.2024.10.024</nowiki></ref>. People with depression often show a tendency to focus more on negative environmental information while ignoring neutral or positive details. This biased attention leads to an imbalanced integration of information across cognitive systems, resulting in predominantly negative memories, interpretations of events, and perceptions of the self, others, and the world. Over time, this creates a self-reinforcing cycle, where the focus on negative information perpetuates depressive thoughts and feelings, sustaining the depressed mood. | ||
=== Treatment === | === Treatment === | ||
Depression, first must be approached as a disorder influenced by environmental factors rather than treated pharmacologically. Jumping to medication to soon may obscure the distinction between external (exogenous) and internal (endogenous) causes. Addressing and eliminating external factors should be | Depression, first must be approached as a disorder influenced by environmental factors rather than treated pharmacologically. Jumping to medication to soon may obscure the distinction between external (exogenous) and internal (endogenous) causes. Addressing and eliminating external factors should be prioritised, followed by an evaluation of potential neurochemical (endogenous) imbalances if symptoms persist.The main points to initially address are: | ||
# '''Healthy diet''' - supplementation of Vitamin D3, tryptophan<ref>'''The effects of dietary tryptophan on affective disorders.''' Arch Psychiatr Nurs. 2015 Apr;29(2):102-7. doi: 10.1016/j.apnu.2014.11.008. Lindseth G, Helland B, Caspers J. Epub 2014 Dec 9. PMID: 25858202; PMCID: PMC4393508. Accessed on 30 Jan 2023 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4393508</ref> and Omega 3, ↓ alcohol consumption. | # '''Healthy diet''' - supplementation of Vitamin D3, tryptophan<ref>'''The effects of dietary tryptophan on affective disorders.''' Arch Psychiatr Nurs. 2015 Apr;29(2):102-7. doi: 10.1016/j.apnu.2014.11.008. Lindseth G, Helland B, Caspers J. Epub 2014 Dec 9. PMID: 25858202; PMCID: PMC4393508. Accessed on 30 Jan 2023 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4393508</ref> and Omega 3, ↓ alcohol consumption. | ||
| Line 24: | Line 25: | ||
==== Pharmacological ==== | ==== Pharmacological ==== | ||
The last step would be to consider taking drug such as a traditional [[Antidepressants|antidepressant]]. Doctors often prescribe the SSRI, fluoxetine as the first port of call however, statistically, they (and all other antidepressants) are only effective by a small margin. It has been found that 54% of adults experience a reduction in symptoms after taking an antidepressant, however 35–40% experience similar improvements after taking a [[placebo]]. This means [[antidepressants]] are only responsible for a decrease in symptoms of around 20%<ref>'''Treatment outcomes for depression: challenges and opportunities.''' Pim Cuijpers, Argyris Stringaris, Miranda Wolpert. Published in the Lancet Psychiatry: February 17, 2020. Accessed on 31 March 2023 via DOI:<nowiki>https://doi.org/10.1016/S2215-0366(20)30036-5</nowiki></ref>. To compound this, the 20% who see some effectiveness are plagued by the fact that about a third of these symptoms return at some point during therapy. | The last step would be to consider taking drug such as a traditional [[Antidepressants|antidepressant]]. Doctors often prescribe the [[SSRI and psychedelics|SSRI]], fluoxetine as the first port of call however, statistically, they (and all other antidepressants) are only effective by a small margin. It has been found that 54% of adults experience a reduction in symptoms after taking an antidepressant, however 35–40% experience similar improvements after taking a [[placebo]]. This means [[antidepressants]] are only responsible for a decrease in symptoms of around 20%<ref>'''Treatment outcomes for depression: challenges and opportunities.''' Pim Cuijpers, Argyris Stringaris, Miranda Wolpert. Published in the Lancet Psychiatry: February 17, 2020. Accessed on 31 March 2023 via DOI:<nowiki>https://doi.org/10.1016/S2215-0366(20)30036-5</nowiki></ref>. To compound this, the 20% who see some effectiveness are plagued by the fact that about a third of these symptoms return at some point during therapy. | ||
=== Relapse === | === Relapse === | ||
Latest revision as of 04:36, 4 February 2025
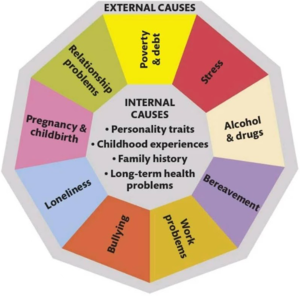
Depression is a mental illness characterized by a persistent low mood, reduced interest in activities, and impaired cognitive function[1]. Its causes are often complex and multifactorial, involving a combination of external (exogenous) factors, such as social influences, and internal (endogenous) factors, including biological and psychological elements like neural wiring and neurochemical imbalances (see Figure 1).
Diagnosis
The diagnosis of depression has traditionally been conducted by psychiatrists or doctors. However, to reduce human error[2][3][4] , there has been a growing shift towards using algorithmic psychometric tests based on yes/no or rating-scale questionnaires. Emerging advancements in the field suggest that voice[5] and facial recognition technology[6] could play a significant role in enhancing diagnostic accuracy in the future.
Cognitive Biases
Cognitive biases are believed to be both a root cause and a symptom of depression, with two primary biases playing a significant role. The first is attention bias, where the mind becomes unconsciously conditioned to focus on negative external stimuli. The second is negativity bias, which involves a tendency to dwell on negative internal thoughts—such as past regrets or future anxieties—as well as unfavorable aspects of the surrounding environment.
Attention acts as a filter, determining which information from our internal thoughts and external environment is processed further[7]. People with depression often show a tendency to focus more on negative environmental information while ignoring neutral or positive details. This biased attention leads to an imbalanced integration of information across cognitive systems, resulting in predominantly negative memories, interpretations of events, and perceptions of the self, others, and the world. Over time, this creates a self-reinforcing cycle, where the focus on negative information perpetuates depressive thoughts and feelings, sustaining the depressed mood.
Treatment
Depression, first must be approached as a disorder influenced by environmental factors rather than treated pharmacologically. Jumping to medication to soon may obscure the distinction between external (exogenous) and internal (endogenous) causes. Addressing and eliminating external factors should be prioritised, followed by an evaluation of potential neurochemical (endogenous) imbalances if symptoms persist.The main points to initially address are:
- Healthy diet - supplementation of Vitamin D3, tryptophan[8] and Omega 3, ↓ alcohol consumption.
- Sunlight - running outside as below can bolster Vitamin D3 as above.
- Exercise - 3+ times a week, the higher the intensity the better, best activity is to run in nature[9][10].
- Sleeping well - by exposing yourself to sunlight you can reset your Circadian Rhythm whilst exercising can also help you sleep.
- Reducing overstimulation - anti rumination, reduce caffeine intake, increase mindfulness and meditation practices.
- Talking - self therapy, counselling, increase social contact.
Psychoplastics
Once exogenous factors have been exhausted, the next step would be to try and rewire the mind to reduce the burden of negativity and attention biases. The easiest way to do this is to induce a pivotal mental state, become neuroplastic and to work in isolation to desensitise the neural pathways associated with endogenous and exogenous factors.
Pharmacological
The last step would be to consider taking drug such as a traditional antidepressant. Doctors often prescribe the SSRI, fluoxetine as the first port of call however, statistically, they (and all other antidepressants) are only effective by a small margin. It has been found that 54% of adults experience a reduction in symptoms after taking an antidepressant, however 35–40% experience similar improvements after taking a placebo. This means antidepressants are only responsible for a decrease in symptoms of around 20%[11]. To compound this, the 20% who see some effectiveness are plagued by the fact that about a third of these symptoms return at some point during therapy.
Relapse
People who have recovered from an episode of depression (whether spontaneously or following the provision of treatment) are at an increased risk of becoming depressed again in the future. This risk can be as high as 60% for people who have experienced one episode, 70% in those who have had two episodes, and 90% in those who have had three previous episodes (American Psychiatric Association, 2000). Psychological therapies delivered following recovery from depression, including CBT, MBCT, and IPT, may reduce risk of relapse after one year by 22%[12].
Trends
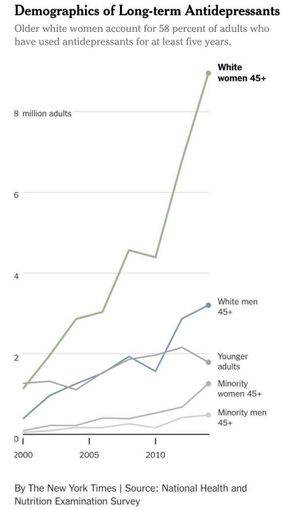
The prevalence of major depression women is a 1.7-fold greater incidence than in men (see Figure 2). Studies suggest that the differential risk may primarily stem from biological sex differences and depend less on race, culture, diet, education and numerous other potentially confounding social and economic factors[13]. There is no conclusive proof that the prevalence of depression is higher in nations where women's socioeconomic standing is noticeably lower than men's than in nations where there may be more equality.[14]
References
- ↑ The association between overweight/obesity and poor cognitive function is mediated by inflammation in patients with major depressive disorder. Xiaofeng Lan, Chengyu Wang, Weicheng Li, Ziyuan Chao, Guohui Lao, Kai Wu, Guixiang Li, Yuping Ning, Yanling Zhou, Journal of Affective Disorders, Volume 313, 2022, Pages 118-125,https://doi.org/10.1016/j.jad.2022.06.073.
- ↑ Rates of Detection of Mood and Anxiety Disorders in Primary Care: A Descriptive, Cross-Sectional Study Monica Vermani, PsyD, Madalyn Marcus, MA. Prim Care Companion CNS Disord. 2011; 13(2): PCC.10m01013. doi: 10.4088/PCC.10m01013. Accessed on 30th November 2022 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3184591/
- ↑ Analysis of Misdiagnosis of Bipolar Disorder in An Outpatient Setting. Shen H, Zhang L, Xu C, Zhu J, Chen M, Fang Y. Shanghai Arch Psychiatry. 2018 Apr 25;30(2):93-101. doi: 10.11919/j.issn.1002-0829.217080. PMID: 29736129; PMCID: PMC5936046. Accessed on 30 November 2022 via: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5936046/
- ↑ Beyond Misdiagnosis, Misunderstanding and Mistrust: Relevance of the Historical Perspective in the Medical and Mental Health Treatment of People of Color. Derek H. Suite, MD, MS; Robert La Bril, MDiv; Annelle Primm, MD, MPH; and Phyllis Harrison-Ross, MD. Accessed on 30 November 2022 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2574307/pdf/jnma00207-0025.pdf
- ↑ Detecting subtle signs of depression with automated speech analysis in a non-clinical sample. König, A., Tröger, J., Mallick, E. et al. BMC Psychiatry 22, 830 (2022). https://doi.org/10.1186/s12888-022-04475-0.
- ↑ Diagnosis of Depressive Disorder Model on Facial Expression Based on Fast R-CNN. Diagnostics (Basel). Lee YS, Park WH. 2022 Jan 27;12(2):317. doi: 10.3390/diagnostics12020317. PMID: 35204407; PMCID: PMC8871079.
- ↑ Woody, M. L., Rohac, R., Cooper, I., Griffo, A., McDonald, N., Spotts, C., Fournier, J., Jones, N., Peciña, M., Young, K., Shivanekar, S., Rengasamy, M., Grafton, B., & Price, R. B. (2024). The Impact of Intravenous Ketamine on Attentional Bias: Probing Mechanisms of Rapid-Acting Antidepressant Effects Across Two Clinical Studies. Biological Psychiatry. https://doi.org/10.1016/j.biopsych.2024.10.024
- ↑ The effects of dietary tryptophan on affective disorders. Arch Psychiatr Nurs. 2015 Apr;29(2):102-7. doi: 10.1016/j.apnu.2014.11.008. Lindseth G, Helland B, Caspers J. Epub 2014 Dec 9. PMID: 25858202; PMCID: PMC4393508. Accessed on 30 Jan 2023 via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4393508
- ↑ Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Ben Singh, Timothy Olds, Rachel Curtis, University of South Australia, Adelaide, Australia; Accessed on 31 March 2023 via the BMJ http://orcid.org/0000-0002-7227-2406
- ↑ The effects of walking in nature on negative and positive affect in adult psychiatric outpatients with major depressive disorder: Kia Watkins-Martin, Despina Bolanis, Stéphane Richard-Devantoy, Marie-Hélène Pennestri, Catherine Malboeuf-Hurtubise, Frederick Philippe, Julie Guindon, Jean-Philippe Gouin, Isabelle Ouellet-Morin, Marie-Claude Geoffroy, A randomized-controlled study, Journal of Affective Disorders, Volume 318, 2022,Pages 291-298, ISSN 0165-0327, https://doi.org/10.1016/j.jad.2022.08.121.
- ↑ Treatment outcomes for depression: challenges and opportunities. Pim Cuijpers, Argyris Stringaris, Miranda Wolpert. Published in the Lancet Psychiatry: February 17, 2020. Accessed on 31 March 2023 via DOI:https://doi.org/10.1016/S2215-0366(20)30036-5
- ↑ Can non-pharmacological interventions prevent relapse in adults who have recovered from depression? A systematic review and meta-analysis of randomised controlled trials. Clinical Psychology Review. Volume 39, July 2015, Pages 58-70
- ↑ Why is depression more prevalent in women? J Psychiatry Neurosci; 40(4): 219–221. doi: 10.1503/jpn.150205 PMCID: PMC4478054PMID: 26107348. Published 2015 Jul. Accessed 8 May 2023 via: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4478054/
- ↑ Country- and individual-level socioeconomic determinants of depression: multilevel cross-national comparison. Br J Psychiatry. 2013;202:195–203. Rai D, Zitko P, Jones K, et al. Published Jan 2018, accessed on 8 May 2023 via https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/country-and-individuallevel-socioeconomic-determinants-of-depression-multilevel-crossnational-comparison/BF4C391FE529178EFF83D8EAED77C138